Anticoagulation Therapy
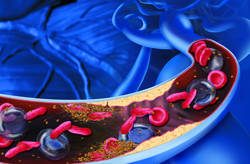
Anticoagulation Therapy is prophylactic (preventive) treatment with medications to reduce the risk of BLOOD clots, broadly including approaches that inhibit various stages of COAGULATION. Anticoagulation therapy is common treatment for a number of cardiovascular conditions including ATRIAL FIBRILLATION, INTERMITTENT CLAUDICATION, DEEP VEIN THROMBOSIS (DVT), PULMONARY EMBOLISM, and VALVULAR HEART DISEASE, and following MYOCARDIAL INFARCTION (HEART ATTACK) and cerebral infarction (ischemic or thromboembolic STROKE). Anticoagulant medications prevent new clots from forming and existing clots from getting larger, though cannot dissolve clots that already exist. Medications that dissolve existing clots are called thrombolytic agents, which have different pharmacologic actions in the body.
The appropriate anticoagulation therapy depends on the reason for the therapy (health condition), the person’s overall health situation, and any other medications the person needs to take. Doctors may prescribe anticoagulation therapy for noncardiovascular reasons such as after orthopedic surgery, particularly JOINT REPLACEMENT. People commonly refer to anticoagulant medications as “blood thinners,” though this is a misnomer because these medications do not alter the blood’s viscosity (thickness).
Antiplatelet Agents
Antiplatelet medications, also called PLATELET inhibitors, slow clot formation by inhibiting PLATELET AGGREGATION. These medications are especially effective in people who have increased risk for CORONARY ARTERY DISEASE (CAD) or thromboembolic stroke. Platelets are the cells in the blood that are first on the scene of any injury in the body. They swarm in response to even the slightest of damage, such as the irritation and INFLAMMATION atheromas cause to the walls of the arteries. When they aggregate, or clump together, they release chemical signals that activate the sequence of events resulting in clot formation. Antiplatelet medications interfere with these chemical signals.
The most commonly used antiplatelet therapy is ASPIRIN THERAPY. Aspirin inhibits PROSTAGLANDINS, chemicals that platelets require to enable them to aggregate or stick together. Aspirin delays clotting by delaying platelet aggregation, which is the first step in the coagulation process. Platelets may come together but not stick, drifting away from each other again before they initiate the clotting process. Other commonly prescribed antiplatelet medications include clopidogrel (Plavix), ticlopidine (Ticlid), dipyridamole (Persantine), and cilostazol (Pletal). These medications may have serious side effects or interact with other medications. Ticlopidine may cause a rare but life-threatening condition, thrombotic thrombocytopenic purpura (TTP), and requires frequent blood tests to monitor for its development.
Clotting Factor Inhibitors
Othe medications act to interfere with the body’s ability to activate blood proteins essential for clotting (CLOTTING FACTORS). The most commonly used oral medication, warfarin (Coumadin), works by blocking one of the steps in the body’s process to produce VITAMIN K. Vitamin K is essential to the metabolic processes that activate clotting factors II, VII, IX, and X. The gastrointestinal tract does not absorb heparin, which is available only in injectable form (intravenous or subcutaneous). Heparin prevents the conversion of prothrombin (clotting factor II) to thrombin, a crucial and early step of coagulation. Both of these medications are NARROW THERAPEUTIC INDEX (NTI) drugs that require very close monitoring to maintain their doses within therapeutic range. Internal bleeding, especially from the gastrointestinal tract, can occur when doses are too high. Excessive bleeding from wounds, such as ACCIDENTAL INJURIES, or from routine dental procedures, such as prophylactic cleaning, is also a risk.
Low molecular weight heparin (LMWH), also only in injectable form, acts similarly to heparin though without many of heparin’s undesired side effects. Several kinds of LMWH, also called fractionated heparin, are available. Each has unique characteristics and though all are LMWH drugs, they are not interchangeable. LMWH products include dalteparin (Fragmin), enoxaparin (Lovenox), and tinzaparin (Innohep). Another injectable medication, fondaparinux (Arixtra), inhibits clotting factor X. Proper site selection and injection technique are important for people who use injectable forms of anticoagulant medications.
Benefits, Risks, and Lifestyle Modifications
Anticoagulant medications, whether antiplatelet or inhibitor, are preventive for blood clots and the health problems blood clots can cause, such as stroke, HEART attack, pulmonary embolism, and DVT. The primary risk of anticoagulation therapy is excessive or prolonged bleeding, which can be serious or life-threatening in some situations. Doctors carefully monitor blood clotting times and other measures to maintain an appropriate therapeutic balance. Spontaneous nosebleed (EPISTAXIS), easy bruising, bleeding from the gums when brushing the teeth, and blood in the stool are signs of excessive anticoagulation that require a doctor’s evaluation.
When on anticoagulation therapy it is important to avoid OVER-THE-COUNTER (OTC) DRUGS such as NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDS) in products for PAIN relief, menstrual cramps, and cold and flu relief, and salicylates such as Pepto-Bismol. These products have mild anticoagulation effects that can cause excessive bleeding in combination with anticoagulation medications. As well, anticoagulation medications interact with numerous other medications and may have side effects, some of which can have serious health consequences.
Many people who are on anticoagulation therapy have underlying cardiovascular conditions that would benefit from lifestyle modifications as well, such as increased physical activity and SMOKING CESSATION. Regularly stretching the muscles throughout the day, especially leg muscles, and walking for 5 to 10 minutes every few hours help keep blood from pooling and clotting.
See also ARRHYTHMIA; GASTROINTESTINAL BLEEDING; LIFESTYLE AND CARDIOVASCULAR HEALTH; THROMBOCYTOPENIA; THROMBOLYTIC THERAPY.