Kidney Donor - Transplant and Living Kidney Donor
What is Kidney Donor
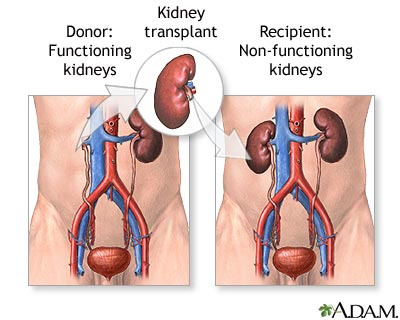
Kidney Donor is an individual who donates his or her KIDNEYS after death or who donates one kidney for live donor transplantation. Kidneys are the organs most commonly transplanted in the United States (other than SKIN and corneas). At present, people waiting for donor kidneys outnumber available kidneys nearly four to one. Between 50,000 and 60,000 people currently await donor kidneys in the United States. A person becomes a potential candidate for KIDNEY TRANSPLANTATION with the onset of END-STAGE RENAL DISEASE (ESRD), a permanent state of renal failure in which the kidneys cannot perform their functions at a level that sustains life.
The donor and the recipient must match in BLOOD TYPE and human leukocyte antigen factors and be negative for antibodies (negative crossmatch). HUMAN LEUKOCYTE ANTIGENS (HLAS) are six inherited proteins (three from each parent) on the surfaces of leukocytes (white BLOOD cells). The more HLAs that match, the greater likelihood the recipient’s body will accept the donor kidney. Even with blood type match and good HLA matching, some people’s immune systems produce antibodies in reaction to the donor’s blood. A negative crossmatch mixes small amounts of the prospective donor’s blood and the recipient’s blood to confirm that there is no ANTIBODY reaction.
Living Kidney Donor
A living donor may be a relative or a stranger to the kidney recipient. In general a living donor must be in overall good health and have two normally functioning kidneys. Some health conditions, such as HYPERTENSION (high BLOOD PRESSURE), chronic LIVER disease, and DIABETES, preclude a person from donating a kidney because the risk is high for developing kidney disease as a consequence of these conditions. People with chronic health conditions generally are not eligible to donate a kidney. There is no greater likelihood of developing kidney disease with only one kidney, and a single kidney can more than adequately accommodate the body’s needs.
The transplant team selects a living donor on the basis of the match between the donor and the recipient. Typically, the recipient’s health insurance pays for the donor’s medical expenses related to the kidney donation, including surgery, hospitalization, and follow-up care. Once selected, the living donor undergoes NEPHRECTOMY, an OPERATION to remove a kidney. There are two options, open nephrectomy and laparoscopic nephrectomy. Either procedure is a major surgery that requires hospitalization and postsurgical recovery time. Though recovery is uneventful for most donors whether they undergo laparoscopic or open nephrectomy, donating a kidney does require time off from work and regular activities.
Laparoscopic nephrectomy requires several small incisions through which the team uses laparoscopy to remove the donor kidney. Though technically more challenging for the transplant team, laparoscopic nephrectomy significantly reduces scarring and recovery time for the donor. Laparoscopic nephrectomy takes three to four hours, with two to three hours in the recovery room while the person returns to full consciousness. Most people who undergo laparoscopic nephrectomy stay one to three days in the hospital after the surgery and require four to six weeks for return to regular activities. Within a year or two, the small scars remaining from the incisions are nearly invisible.
Open nephrectomy requires a single large incision and takes two to three hours, with two to three hours in the recovery room to return to full consciousness. Most people who undergo open nephrectomy stay three to five days in the hospital after the surgery and need six to eight weeks for return to regular activities. The SCAR from the incision begins to fade in about a year.
The transplant team immediately performs the transplantation surgery to place the donor kidney into the recipient. Only the intended recipient may receive the living donor kidney; there are no waiting list requirements for live donor kidney transplantations. Living donor kidney transplants have a higher long-term success rate than cadaver donor kidney transplants.
Cadaver Donor
Cadaver donor kidneys come from the bodies of deceased persons who died of causes not related to kidney function, had healthy kidneys at the time of death, and signed documents affirming their desires to donate their organs after their deaths. Family members may make the decision about organ donation when the person dies without organ donor documentation. Organ donation can proceed only when the appropriate assessments certify the person has suffered BRAIN DEATH.
UNIVERSAL DONOR CARD
Most states honor the universal donor card, a wallet-size document affirming a person’s intent to donate his or her organs upon death, as a legal document. Many states incorporate the universal donor card into the driver’s license.
A transplant team removes donor kidneys using sterile surgical technique and a procedure similar to nephrectomy (surgical removal of a kidney such as to treat RENAL CANCER), carefully preserving the blood vessels and URETER. After removing the kidneys, called organ harvesting, the transplant team places them in a cold solution that can sustain them for 36 to 48 hours and sutures closed the incisions made to gain access to the kidneys. The organ-processing procedure includes screening of the donor kidneys for any diseases they could convey to the recipient. In the United States an independent organization called the United Network for Organ Sharing (UNOS) oversees the collection and distribution of all cadaver donor organs in compliance with strict guidelines intended to ensure equity in the process of matching donor organs with recipients. The transplant surgery must take place within 36 to 48 hours of the kidney’s harvesting, sooner if possible.
See also ORGAN TRANSPLANTATION; QUALITY OF LIFE; SURGERY BENEFIT AND RISK ASSESSMENT.