Coronary Artery Bypass Graft (CABG)
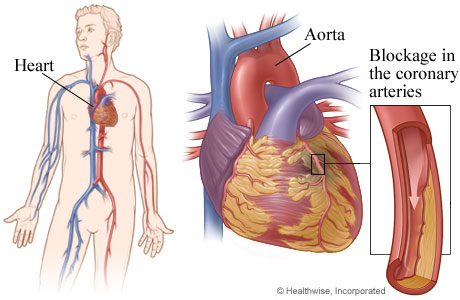
Coronary Artery Bypass Graft (CABG) is a surgical OPERATION to replace diseased CORONARY ARTERIES supplying the HEART with BLOOD. Cardiovascular surgeons began performing CABG to treat severe CORONARY ARTERY DISEASE (CAD), typically following HEART ATTACK, in the 1960s. The operation became feasible with refinements in CARDIOPULMONARY BYPASS technology and surgical technique. In the ensuing decades CABG has become one of the most frequently performed operations in the United States, with surgeons performing more than 300,000 a year. The surgeon may use CABG to replace one to five coronary arteries; three or four is most common (triple or quadruple bypass). The most frequently bypassed coronary arteries are the left anterior descending (LAD), which traverses the front of the heart; the circumflex, which wraps around the heart; and their respective branches.
Weighing the Benefits and Risks
Whether Coronary Artery Bypass Graft (CABG) is an appropriate treatment choice depends on numerous variables that include the person’s age and general health status, degree and extent of occlusion in the coronary arteries, and the presence of other CARDIOVASCULAR DISEASE (CVD). Variables that strongly influence the procedure’s success include lifestyle factors such as cigarette smoking, body fat and weight, physical inactivity, and dietary habits. Other health conditions that affect HEALING, such as DIABETES, are also important considerations, as are conditions affecting the LUNGS such as CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD).
Now that several million Americans have had CABG and researchers have accumulated data spanning four decades, evidence is emerging that calls into question the ultimate effectiveness of CABG in preventing deaths due to CAD. A number of studies indicate that CABG may not extend LIFE EXPECTANCY or improve QUALITY OF LIFE to the degree cardiologists and others believe it does. Researchers continue to explore all dimensions of this debate.
Coronary Artery Bypass Graft (CABG) - Surgical Procedure
The typical Coronary Artery Bypass Graft (CABG) takes 75 to 90 minutes for the surgeon to perform. The first steps in CABG are to open the chest, initiate cardiopulmonary bypass, and stop the heart. The preferred approach for the grafts is to use the person’s own blood vessels to reconstruct the occluded coronary arteries. The most viable vessels for this purpose are the right and left internal mammary arteries, which the surgeon exposes when opening the chest to perform the CABG. These arteries are ideal because they do not require additional incisions to obtain, and there is a good supply of arterial circulation to replace them. As well, the mammary arteries are about the same size as the coronary arteries, allowing them to accommodate the demands the coronary circulation will place on them. The surgeon may be able to craft two and sometimes three grafts using both internal mammary arteries. Because of its size and importance to coronary circulation, the LAD is first in line for an arterial graft. The surgeon needs about 6 inches of graft for each coronary ARTERY bypass created.
When the Coronary Artery Bypass Graft (CABG) involves more coronary arteries than the mammary arteries can accommodate, the surgeon typically harvests a segment of the saphenous VEIN from the leg, which requires an incision in the groin. Though effective enough, the saphenous vein graft is less than ideal for service as a coronary artery and is more prone to postoperative complications. Although its size makes it a sturdy vessel, the saphenous vein lacks the muscular construction of an artery and has a greater risk of collapsing or closing than does an arterial graft. As well, some people have residual edema and other complications after surgery in the leg from which the surgeon harvests the vein. An alternative practice is to instead harvest segments of arteries from elsewhere in the body for which there is relatively redundant circulation (other arteries to provide blood supply), such as the radial artery or the brachial artery in the arm. When autografts such as these are not possible, the surgeon may use a synthetic material specially treated to resist clotting. However, synthetic grafts are not as reliable as autografts.
The surgeon sutures (sews) one end of the graft into the AORTA above the occlusion and the other end into the coronary artery below the occlusion to establish the bypassed path of circulation. The surgeon does this for each occluded coronary artery. When the internal mammary artery provides the graft, the surgeon needs only to suture at the distal end because the proximal end is already in place. The diseased coronary artery segments stay in place though will no longer carry blood. When finished bypassing the occluded coronary arteries, the surgeon restores blood circulation through the heart and restarts the heart with a chemical solution or an electrical charge. After making sure the grafts are intact and not leaking, the surgeon closes the chest. Wires hold the ribs and sternum in place, while sutures and staples close the layers of MUSCLE and SKIN.
Risks and Complications of Coronary Artery Bypass Graft
Coronary Artery Bypass Graft (CABG) entails numerous risks and complications. Though its frequency gives the perception that it is a routine operation, CABG is a significant major surgery during which the surgeon places the person on cardiopulmonary bypass, cuts through the breastbone and several ribs to expose the heart, stops the heart to reconstruct the coronary arteries, and then restarts the heart and closes the chest. Each step carries its own risks. Collectively, the major risks of CABG include
- air emboli (air bubbles that get into the bloodstream and create blockages), causing heart attack, STROKE, or PULMONARY EMBOLISM
- excessive bleeding during surgery
- bleeding when the surgeon restores circulation through the heart
- inability to restart the heart
- inability to wean from the cardiopulmonary bypass machine when surgery is done
- postbypass neurologic damage with residual consequences that may include cognitive dysfunction, memory impairment, and physical dysfunctions such as localized loss of feeling or function
- rapid restenosis (within six months) of the grafts
- collapse of venous grafts
Improved technology is making other treatment options, notably ANGIOPLASTY, increasingly viable. Some studies suggest that angioplasty with STENT placement, which is significantly less invasive and less expensive than CABG, is equally effective for multiple vessel CAD and in a good number of people lasts as long as CABG. On the other side of the debate, clinical results with allarterial grafts for CABG show increased reliability. As well, advances in microsurgery and endoscopic surgery are making MINIMALLY INVASIVE CARDIOVASCULAR SURGERY increasingly feasible, allowing surgeons to perform minimally invasive direct coronary artery bypass (MIDCAB) procedures using multiple small incisions rather than fully opening the chest. Some surgeons are using “offpump” procedures, in which the heart continues to function during the operation, to reduce the risk for neurologic and pulmonary side effects. Others are combining angioplasty with MIDCAB in a procedure called hybrid CABG. Researchers and surgeons continue to study these approaches and methods, comparing outcomes to determine the most appropriate options.
Outlook and Lifestyle Modifications
Most people spend three to five days in the hospital and another four to eight weeks recovering at home before making a full return to regular activities. The improvement in cardiovascular function is apparent immediately for most people. Cardiologists typically recommend cardiac rehabilitation for people who have had CABG, to help establish a structure for any necessary lifestyle modifications. The clinical standard for postoperative care now includes medications such as beta blockers and statins, drugs to stabilize HEART RATE and lower cholesterol blood levels, respectively. Statins also appear to have a stabilizing and strengthening action on the heart, with numerous clinical studies showing that people who take statins following CABG have significantly fewer complications, notably heart attack, after surgery. Cardiologists also urge people to eat nutritiously, get a minimum of 30 minutes of physical exercise each day, stop smoking, and lose weight to achieve a healthy BODY MASS INDEX (BMI). Most people experience complete and uneventful recovery from surgery and return to work and the recreational activities that interest them.
See also CARDIOVASCULAR DISEASE PREVENTION; COGNITIVE FUNCTION AND DYSFUNCTION; POSTOPERATIVE PROCEDURES; PREOPERATIVE PROCEDURES; SMOKING CESSATION; SURGERY BENEFIT AND RISK ASSESSMENT.