Heart Transplantation surgery
What is Heart Transplant
Heart Transplantation is the replacement of a diseased HEART with a healthy heart from a deceased donor. Heart transplantation is a therapeutic option for severe CONGENITAL HEART DISEASE such as hypoplastic left heart syndrome (HLHS) as well as hypertrophic CARDIOMYOPATHY and end-stage HEART FAILURE. South African heart surgeon Christiaan Barnard (1922-2001) performed the first human heart transplantation in 1967, when he replaced the badly diseased heart of 53-year-old Louis Washkansky with the healthy heart of 25-year-old Denise Darvall who died in an accident. Though Washkansky lived only 18 days with the new heart, the OPERATION catapulted cardiovascular medicine into a new era. Today cardiovascular surgeons perform about 2,200 heart transplant operations a year in the United States. More than 70 percent of donor heart recipients live at least 5 years; the longest survival is 24 years.
DONOR HEART SHORTAGE
More than 4,000 people wait on the donor HEART list, yet donor hearts will be available for little over half of them. Many people who could be heart donors are not. Surgeons must place the donor heart in the recipient within four hours of the donor’s death. Because many people have not made decisions in advance about organ donation, the time it takes to obtain the family’s permission may make it too late to use the heart. There is no cost to the donor’s family for removal of donated organs.
Heart transplant recipient criteria
Though many people may become critically ill with CARDIOVASCULAR DISEASE (CVD), heart transplantation is a viable option primarily for end-stage heart failure. Health experts estimate that heart transplants could save the lives of 25,000 or more people each year who currently die as a result of heart failure, though the severe shortage of donor hearts restricts heart transplantation to people who are dying from heart failure yet are otherwise healthy-people who have both great need and great potential for survival. Conditions that may result in heart transplantation include
- end-stage heart failure for which medical therapies are ineffective, typically resulting from inoperable CORONARY ARTERY DISEASE (CAD), inoperable VALVULAR HEART DISEASE, and cardiomyopathy
- life-threatening ARRHYTHMIA that does not respond to other treatment
- inoperable congenital malformations of the heart, such as HLHS and tetralogy of Fallot, when surgical reconstruction of the heart either fails or is not likely to be successful
Though numerous clinical criteria establish the severity of cardiovascular status, typically LEFT VENTRICULAR EJECTION FRACTION (LVEF) that falls below 25 percent is the decisive factor. LVEF represents the percent of blood in a full left ventricle that the heart pumps into the body with each contraction of the left ventricle. The amount of blood that enters the body is the stroke volume. A normal LVEF is 55 percent or higher; an LVEF of 40 percent is moderately debilitating. At 25 percent, there are symptoms of cardiovascular distress (such as shortness of breath and ANGINA PECTORIS) even at rest and the person is unable to perform most physical activities.
As well, there are general eligibility criteria to ensure optimal chance for survival after transplantation. These general criteria for heart transplantation include
- expectation of one year or less survival
- age 65 or younger (though an older person who meets all other criteria may be accepted as a recipient)
- otherwise good health
- capable of and willing to comply with lifelong medical care
Various health circumstances tend to preclude consideration for heart transplantation, though they are not absolute. Called comorbid conditions, these include
- INSULIN-dependent DIABETES with NEPHROPATHY, NEUROPATHY, or RETINOPATHY (damage to KIDNEYS, nerves, or eyes)
- primary irreversible kidney disease (not related to cardiovascular disease)
- primary irreversible LIVER disease such as CIRRHOSIS (not related to cardiovascular disease)
- cancer within the previous five years (except SKIN)
- PERIPHERAL VASCULAR DISEASE (PVD) with symptoms such as INTERMITTENT CLAUDICATION
- TRANSIENT ISCHEMIC ATTACK (TIA)
- PRIMARY PULMONARY HYPERTENSION (PPH), CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD), EMPHYSEMA, or severe ASTHMA
- OBESITY
Though none of these criteria is absolute, because of the extreme limited availability of donor hearts cardiologists must be able to justify exceptions. Heart transplantation centers set their own criteria, which may be more or less stringent than the general criteria. Many heart transplantation centers are reluctant to approve individuals who are not likely to maintain the rigorous therapeutic and lifestyle regimens necessary following transplant. In infants and children, heart transplantation is an option for nonsurvivable major congenital anomalies. The shortage of donor hearts severely limits heart transplantation in infants, however.
The donor heart
The United Network for Organ Sharing (UNOS) maintains donor lists for all transplant circumstances (except corneas and SKIN) in the United States. UNOS coordinates the acquisition and distribution of donor organs according to strict guidelines and policies that direct available organs to the sickest people on the waiting lists for whom criteria match. Regional transplantation centers carry out the acquisitions and distributions. People waiting for heart transplants must be available 24 hours a day and must be able to reach their transplantation centers within two hours.
The donor’s BLOOD TYPE must be the same as the recipient’s, and the donor and recipient need to be similar in body size and weight. The heart of a donor who is six feet, four inches tall will not fit in the chest cavity of a recipient who is five feet, three inches tall. Similarly, the heart of a small donor cannot meet the cardiovascular needs of a large recipient. Gender, race, and ethnicity do not matter. The donor’s heart must be healthy, and the donor must be under age 65 and free from serious or communicable diseases. Most donor hearts come from people who lose their lives in accidents that cause irreversible, overwhelming BRAIN damage. A specialized surgical team carefully harvests the heart in the operating room, after certifying brain death though while cardiovascular function continues, and places the heart in a cold electrolyte solution to preserve it during transport to the recipient’s medical center. The heart remains viable for four to six hours.
Heart Transplantation - Surgical Procedure
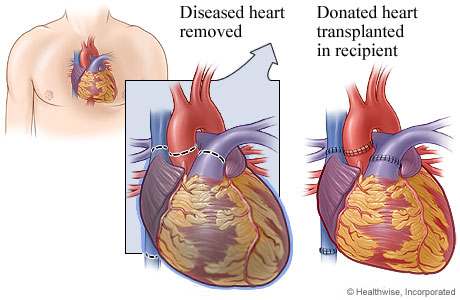
The heart transplant operation typically takes three to five hours. The surgeon opens the chest with a large incision lengthwise over the STERNUM and cuts the sternum with a saw to open the chest. After placing the person on CARDIOPULMONARY BYPASS (mechanical oxygenation and circulation of the blood), the surgeon removes the diseased heart. There are several methods for doing this; the most common is to cut away all of the heart except the back walls of the atria to preserve the connections to their blood vessels (the superior VENA CAVA, inferior vena cava, and pulmonary VEIN). Respectively, the surgeons cut away the back of the donor heart to match and suture the donor heart into place beginning with the left atrium. The great arteries the AORTA and the pulmonary ARTERY-are the final structures the surgeon attaches. The heart spontaneously begins to beat when the surgeon restores blood flow. The surgeon closes the sternum with wire to hold it together while it heals, and closes the outer chest tissues with sutures or staples. Most people remain in the hospital up to 10 days following surgery.
Heart Transplantation Risks and Complications
Heart transplantation entails numerous risks and complications during (operative) and following (postoperative) the surgery. Operative risks include bleeding, air embolism (air that escapes into the bloodstream from the cardiopulmonary bypass), unexpected anatomic incompatibilities (the donor heart does not “fit”), and inability to restore cardiac function. The most significant complications following heart transplantation, which also account for the greatest number of deaths, are INFECTION and rejection. Arrhythmias and other dysfunctions of the heart sometimes occur, though typically respond to medications. Occasionally the transplanted heart fails to function, a circumstance called graft failure. Immediate retransplantation is generally the only treatment.
People who have transplanted hearts are vulnerable to rapidly progressive CAD, HYPERTENSION, and arrhythmias. The transplanted heart is denervated-though it contains its own conductive NERVE network to convey electrical pacing impulses, it does not have nerves connecting it to the body’s sympathetic nerve pathways. Normal NERVOUS SYSTEM mechanisms (the sympathetic nerve pathways) that typically regulate HEART RATE and cardiac workload are not functional in the transplanted heart, though in some people reinnervation occurs over time. The absence of sympathetic nerve pathways also means the person does not experience angina pectoris, a primary symptom of CAD and ISCHEMIC HEART DISEASE (IHD). This increases the risk for silent HEART ATTACK. Cardiologists closely monitor the transplanted heart for any signs of CAD, and also routinely prescribe lipid-lowering medications to help prevent CAD from developing.
Other long-term risks include an increased risk for cancer, most commonly skin and lymphatic, because of the IMMUNOSUPPRESSIVE THERAPY. Infection and rejection remain risks as well. Rejection can be acute (come on suddenly and severely) or chronic (persist in a low-grade fashion over time, or come and go). Many cardiologists believe the accelerated CAD process also results from immunosuppression rather than the conventional factors.
Heart Transplantation Outlook and Lifestyle Modifications
Most people remain hospitalized for 5 to 10 days after the transplant operation, while the new heart stabilizes and the surgical wounds start to heal. During this time doctors initiate IMMUNOSUPPRESSIVE THERAPY, ANTICOAGULATION THERAPY, and various medications to support the heart’s function during early HEALING. All transplant recipients will need to take IMMUNOSUPPRESSIVE MEDICATIONS for the remainder of their lives to prevent their bodies from rejecting the donor organ.
Most heart transplant recipients will continue taking other cardiovascular medications to support cardiovascular efficiency. The transplanted heart’s denervation affects its ability to adjust to changing cardiovascular needs in the body, such as with exercise. Many people require a PACEMAKER after transplantation to maintain an adequate heart rate and appropriate heart rhythm. Heart transplantation requires lifetime medical follow-up, usually annual CARDIAC CATHETERIZATION and other diagnostic procedures to assess the heart’s function.
Most heart transplant recipients return to their regular work and leisure activities, including sexual activity, gradually over two to three months. The cardiologist may restrict certain kinds of strenuous physical activity depending on the heart’s ability to respond to the body’s increased oxygen needs. The healing process is generally quite rapid as full cardiovascular function returns the body to its normal function. CARDIAC REHABILITATION helps restore the body to a level of physical STRENGTH and AEROBIC FITNESS that further supports cardiovascular health. Moderate daily physical exercise (such as walking), nutritious eating habits, and total abstinence from smoking are essential.
See also CARDIOVASCULAR DISEASE PREVENTION; MEDICATIONS TO TREAT CARDIOVASCULAR DISEASE; OPEN HEART SURGERY; PHYSICAL EXERCISE AND CARDIOVASCULAR HEALTH; QUALITY OF LIFE; SEXUAL ACTIVITY AND CARDIOVASCULAR DISEASE; TRANSMYOCARDIAL LASER REVASCULARIZATION (TMLR); VENTRICULAR ASSIST DEVICES (VADS).