Decubitus Ulcer - staging, symptoms and treatment
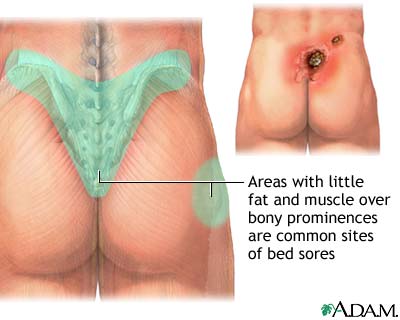
Decubitus Ulcer - An erosion in the SKIN that results from the pressure of remaining in one position for an extended period of time, commonly called a bedsore or pressure sore. The extended pressure deprives the tissue of blood circulation, allowing cells to die and the tissue to break down. Tissues over areas where the bones are near the skin are most vulnerable, such as the hips, ankles, heels, elbows, shoulders, base of the spine, and back of the head. Decubitus ulcers are a specific risk for people who have debilitating conditions or injuries that limit their mobility, particularly elderly individuals in extended-care facilities. MALNUTRITION and age-related changes to the skin result in fragility that makes the skin more susceptible to damage.
Often, measures such as frequent changes of position and soft surfaces to shelter the skin at contact points can prevent decubitus ulcers. Within contemporary quality of care standards and guidelines in health care, decubitus ulcers raise questions as to whether providers and facilities are delivering appropriate care. Undetected or untreated decubitus ulcers can result in significant tissue loss and threaten overall health. Once established, a decubitus ulcer requires aggressive medical intervention to limit permanent tissue damage and restore healthy skin.
Staging of Decubitus Ulcers
| Clinical Staging of Decubitus Ulcers | ||
|---|---|---|
| Clinical Stage | Presentation | Tissue Penetration |
| stage 1 | nonblanching red area | superficial layers of skin (epidermis, first layer of dermis) |
| stage 2 | BLISTER or open sore | full skin (epidermis and full thickness of dermis) to the underlying FASCIA |
| stage 3 | craterlike sore that oozes or bleeds; damaged or necrotic (dead) SKIN; fatty tissue damage to underlying tissues | through the skin and fascia, into the supportive connective and |
| stage 4 | deep ulcer that bleeds; extensive skin and tissue destruction and necrosis | through the skin, fascia, and underlying structures into adjacent MUSCLE, TENDON, and LIGAMENT, and JOINT |
Symptoms of Decubitus Ulcer and Diagnostic Path
The symptoms of decubitus ulcer depend on its stage of development. Health-care providers classify decubitus ulcers on a scale of 1 to 4, with stage 1 being the slightest level of damage and stage 4, the most significant. PAIN is not an effective measure of a decubitus ulcer’s severity as the damage to the skin and underlying tissues may destroy NERVE endings. Doctors diagnose a decubitus ulcer on the basis of its appearance.
Decubitus UlcerTreatment Options and Outlook
The first and most urgent action in treating decubitus ulcers is to relieve all pressure on the area. This may include using pillows, cushions, pads, and other items to support the body in positions that do not put pressure on or near the ulcer. Additional treatment may include regularly cleansing the ulcer to prevent INFECTION, or ANTIBIOTIC MEDICATIONS to treat infection that already exists. Deep ulcers (stage 3 and especially stage 4) often require surgical débridement (removing dead and damaged tissue under anesthetic).
Recovery depends on the stage of the ulcer and the general health condition of the person. With early and aggressive intervention, recovery can be complete with minimal permanent tissue damage. Stage 2 and stage 3 ulcers generally heal with some loss of tissue and scarring. Stage 4 ulcers are extensive wounds that may require multiple débridements and long-term treatment by a WOUND CARE specialist. When debilitation is longterm or permanent, the risk for recurring decubitus ulcers is high.
Decubitus Ulcer Risk Factors and Preventive Measures
People whose health conditions limit their ability to move parts of their bodies or confine them to wheelchairs or bed have very high risk for decubitus ulcers. Preventive measures include
- position changes every two hours when in bed and every 15 minutes when sitting in a chair or wheelchair
- air mattress with alternating compartments or air flotation mattress
- eggshell mattress or seat cushion
- sheepskin pads over bony protuberances such as the heels and elbows
- active movement at least four times a day when possible and passive range of motion exercises when active movement is not possible
- frequent (at least daily) inspection of areas vulnerable to pressure
- diligent skin hygiene, including daily cleansing and complete drying
Prompt intervention at the earliest signs of a decubitus ulcer can prevent extensive or permanent tissue damage.
See also AGING, INTEGUMENTARY CHANGES THAT OCCUR WITH; CELLULITIS; EPIDERMOLYSIS BULLOSA; GANGRENE; SCAR; SPINAL CORD INJURY; TRAUMATIC BRAIN INJURY (TBI).