Osteomyelitis - definition, symptoms and treatment
What is Osteomyelitis and Definition
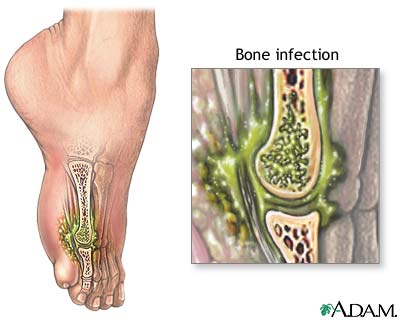
Osteomyelitis - An INFECTION of the BONE. Typically the infection starts elsewhere in the body and spreads through the BLOOD circulation to the bone, though may originate in the bone as a complication of surgery on the bone (such as open reduction of a FRACTURE or JOINT REPLACEMENT). Bacterial infection causes most osteomyelitis, though other pathogens such as fungi (yeast) may also be responsible. The long bones in the leg are the most common locations for osteomyelitis in children; osteomyelitis in adults tends to settle in the hip or pelvis.
Symptoms of Osteomyelitis and Diagnostic Path
Symptoms of osteomyelitis include
- PAIN from the area of the infection
- swelling in the area of the infection
- FEVER
- generalized discomfort and sense of not feeling well
The diagnostic path begins with a comprehensive medical examination and PERSONAL HEALTH HISTORY to identify any recent infections, injuries, or surgeries. X-RAY may show the area of infection, though other imaging procedures such as bone scan or MAGNETIC RESONANCE IMAGING (MRI) often produce more complete information. Biopsy of the site confirms the diagnosis and can identify the responsible PATHOGEN. Blood tests such as complete blood count (CBC) are likely to show elevated white blood cell (WBC) count and other changes in the blood when there is an infection present.
Osteomyelitis Treatment Options and Outlook
Surgical debridement (an OPERATION to clean pus and damaged tissue from the infected area) and ANTIBIOTIC MEDICATIONS administered intravenously are the first course of treatment for osteomyelitis. Once the infection is under control, the doctor may switch to oral antibiotics. The course of antibiotic treatment may extend six weeks or more, depending on how well the infection responds.
Infections in the bone are particularly hard to treat because the bone’s blood circulation does not deliver antibiotic medications to the bone very effectively. The infection may cause an ABSCESS (pocket of pus) that in turn causes the death of bone tissue. When such a scenario unfolds, the osteomyelitis becomes chronic and may destroy considerable bone tissue. It may be necessary for the orthopedic surgeon to create a surgical wound over the site of the infection to clean it and irrigate the area.
Acute osteomyelitis that responds to antibiotic medication may heal without complications. Chronic osteomyelitis, particularly with abscess, may have a less favorable outcome with extended antibiotic therapy necessary for several months. Several surgical operations may be necessary to clean the infection site and prevent abscesses from forming. The surgeon may leave the wound open or insert a drain to facilitate HEALING. Long-term chronic osteomyelitis can cause permanent damage to the structure of the bone. When chronic osteomyelitis accompanies joint replacement, it may be necessary to remove the prosthesis until the infection heals. The treatment of last resort is AMPUTATION.
Risk Factors and Preventive Measures
People at particular risk for osteomyelitis are those who have DIABETES or who are on hemodialysis for END-STAGE RENAL DISEASE (ESRD). Trauma to the bone, such as open fracture or surgery, also increases the risk for infection. Prevention is not always possible, though using measures to appropriately care for wounds and respond to early symptoms such as pain can keep the infection contained enough for antibiotic therapy to be effective.